


Established by the American Diabetes Association, we observe National Diabetes Month every November. If it seems odd to dedicate an entire month to a single disease, consider this – the U.S. Department of Health and Human Services reports “one in 10 Americans have diabetes” and “another 84 million adults in the United States are at high risk of developing type 2 diabetes.”
Combined, over 114 million adults are diabetic or prediabetic! Given that the population of the U.S. was 323 million in 2016, we’re talking about a disease that affects or could affect one-third of the general population. That probably makes it easy to see why diabetes merits its own month!
Diabetes causes health problems throughout the body, including down in the feet. This can be attributed to the fact elevated sugar levels damage nerves and impair the body’s immune system.
If you don’t take proper care of your feet, you have an increased risk for a couple of very serious medical complications – Charcot foot and diabetic ulcers.
When we say, “proper care,” we don’t mean you occasionally take some effort or give your feet attention only every once in a while. You need to be vigilant with your foot care on a daily basis. The good news is this doesn’t have be extremely complicated or time-consuming.
From a general perspective, daily foot care for diabetic feet is centered on protecting your lower limbs and identifying problems at the earliest opportunity. More specifically this entails measures like:
These are all important measures you need to take, but even more so is to come see us here at our Bloomington, IN office at the earliest possible opportunity if you realize something is wrong.
For more information, or to schedule an appointment, call us at (812) 333-4422.
Podiatrists have two different general courses of treatment to help our patients overcome pain and restore functionality to feet and ankles – surgical and nonsurgical. Between the two, conservative treatments are typically the preferred course of action (for both us and our patients!). If we can fix your problem without having to use a surgical procedure, we will.
Of course, there times when conservative care isn’t the best approach. Fortunately, we have various foot and ankle surgeries to handle the job, when needed.
An emergency situation, obviously, can be a clear indication surgery is needed. If you fracture a foot bone that pierces through the skin, you need to seek immediate medical care. While in the emergency room, surgery will be used to put the bone back in place and close the wound. Not all situations are as obvious, however.
Understanding if it’s time for you to consider surgery really comes down to a couple of matters:
The good news about foot and ankle problems is the fact nonsurgical treatment is often quite effective at providing relief from pain and allowing natural healing. Before recommending surgical intervention, we may try to treat the injury or condition using time-proven methods like immobilizing the area (braces, splints, etc.), creating a stretching program, or prescribing medication or orthotic therapy.
Whereas these are often able to get the job done, this isn’t always the case – and that’s one way how you will know it might be time for surgery.
In the cases of severe pain (or dysfunction), there may be something seriously wrong from a structural perspective. To correct structural abnormalities—either inherited or as the result of injury—or arthritic conditions that are causing severe pain, we may recommend a foot or ankle surgery to resolve the problem and provide relief.
For certain conditions (especially toe deformities), we may be able to address symptoms with the use of nonsurgical treatment. When caught early, this can potentially be the case for bunions and hammertoes. These issues, though, are progressive – which means they worsen over time when left untreated and cannot be corrected without surgical intervention.
If you have been living with a bunion or hammertoe for a long time, it’s possible the condition has progressed to a point surgery is your best chance at finding optimal pain relief.
Perhaps the best way to know if it’s time to consider undergoing surgery in a foot or ankle is by our professional recommendation. We do not perform surgeries if they aren’t necessary, so you can trust us to steer you in the right direction when it comes to your treatment.
No matter what type of treatment is best—whether conservative or surgical—you will find the care you need at the office of Kevin J. Powers, DPM. For more information on the services we provide, or to request an appointment for consultation or treatment, give our Bloomington, IN office a call at (812) 333-4422 and one of our team members will be glad to help!
An Achilles tendon rupture is a painful injury that can sideline you for a long time. Even worse, it might never fully heal in the correct way if you don’t get the right treatment. Fortunately, you can start finding the treatment you need at our Bloomington office.
The injury itself takes place when an Achilles tendon sustains a sudden increase in stress. This can happen during intense sports participation, but also following a fall from height or by unexpectedly stepping into a hole in the ground.
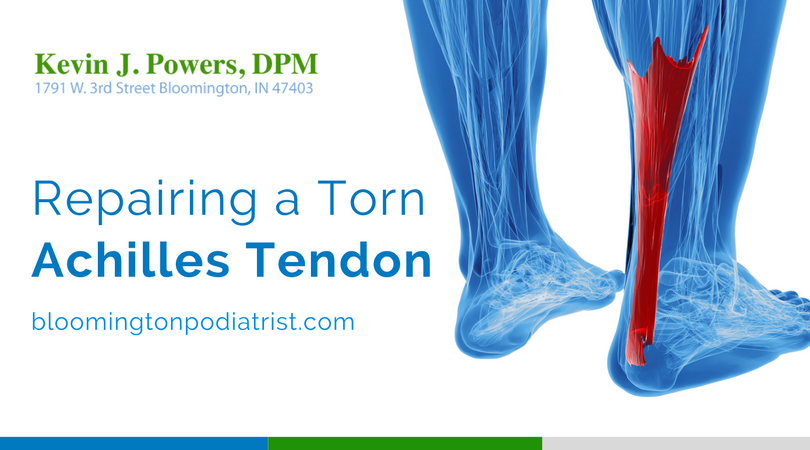
A torn Achilles tendon can be a big problem on account of its functionality and purpose. Your Achilles connects your calf muscle to your heel bone. In doing so, it enables you to raise your heel off the ground (which is obviously important for stepping and jumping).
To handle the tremendous forces needed to propel the body forward in an explosive manner, this particular tendon is the strongest. Of course, it’s not infallible and tends to be the most commonly injured tendon in the human body.
At the time of the injury, you may feel a pop or snap, and then a sharp pain in the back of your ankle and lower leg. In all likelihood, this will affect your ability to walk and rise up onto your toes. Additionally, you will experience a swelling in the back of your leg, between the calf and your heel.
Depending on the nature of your case, proper treatment for your Achilles tendon rupture will be either conservative or surgical. In cases where nonsurgical treatment is the recommended course of action, we may prescribe rest, ice, pain relievers, and immobilization.
In the case of surgical treatment for an Achilles tendon rupture, the goal is to reattach the torn ends of the connective tissue. This can be an important step for ensuring the damaged tissue heals correctly and reducing the risk of chronic pain.
After your surgery, you’ll wear a cast or special boot for a while, and we will monitor your progress. Once your foot is safe to move, you’ll begin physical therapy to help your Achilles regain function and increase its range of motion. After your tendon is completely healed, you’ll be able to ease back into normal activities and routines.
Achilles tendon ruptures can be prevented by stretching and strengthening calf muscles, mixing up your exercises, and gradually increasing training intensity. With this in mind, be sure to stretch properly before games or practices. Also, ease into athletic completion with a progressive workout routine instead of jumping right into intense competition.
For more information on Achilles tendon repair—or any of the foot and ankle services we provide—contact our office by calling (812) 333-4422. If you’d prefer, please feel free to take a moment right now and connect with us via our online form found here on our website.
 There are several different possible explanations for ball of foot pain. If you are experiencing unusual sensations—like feeling as though you are standing on a pebble in your shoe (when there isn’t anything in there)—it is quite possible you have developed a nerve condition called Morton’s neuroma. If the pain or abnormal sensations are coming from between the bases of the third and fourth toes, it’s more likely this is exactly what is plaguing you.
There are several different possible explanations for ball of foot pain. If you are experiencing unusual sensations—like feeling as though you are standing on a pebble in your shoe (when there isn’t anything in there)—it is quite possible you have developed a nerve condition called Morton’s neuroma. If the pain or abnormal sensations are coming from between the bases of the third and fourth toes, it’s more likely this is exactly what is plaguing you.
Never heard of a neuroma before? Well, this is a condition wherein physical damage of some kind has led to a thickening of nerve tissue. The resulting bundle of nerves can misfire, which is the source of pain and unfamiliar sensations.
When you have a Morton’s neuroma, one thing is certain – you will want relief. In some cases, treating this condition is simply a matter of switching your footwear. This means your starting point for finding relief is to choose shoe models that have wide, deep to boxes (the front part of a shoe). Avoid ones that are tight, and especially high heels.
In addition to shoe changes, part of our initial treatment for a Morton’s neuroma may include using anti-inflammatory medications to reduce swelling in the area and relieve pain. Possible options include ibuprofen, naproxen, and other nonsteroidal anti-inflammatory drugs (NSAIDs). For optimal pain relief and safety, make sure to follow our dosage recommendations and give us a call if you have any questions.
Other conservative treatment options include shoe insoles, rest and ice. Insoles are usually of minimal benefit, but there is a chance they will help and may be worth trying. Reducing your usual physical activities—and especially high-impact ones like jogging, running, dancing, and sports played on hard surfaces—gives your feet a much-needed break. You don’t have to completely abandon all exercises, though! Instead of being inactive, use low-impact activities like cycling and swimming.
When conservative treatment doesn’t provide the relief you hope to see, it may be time to explore injection therapy or surgery. Some patients are treated effectively with the use of corticosteroid injections. For others, the nerve will need to be decompressed. Some doctors advocate removing the nerve, but this is a mistake!
Morton’s neuroma is one of the many lower limb conditions we treat at our Bloomington office, which means there is no need to suffer from any foot or ankle pain! Instead, come in and see us for the effective care you deserve. Contact us today for more information by filling out the online form found here on our website or simply give us a call at (812) 333-4422.

The balls of your feet are like unsung heroes – they help you push off when you step, stand on your tippy toes, jump, and more, but they’re never paid much attention. Of course, all that changes when they start hurting and hindering you from doing things you enjoy!
Pain in the balls of your feet can result from a number of causes, but the two main culprits are metatarsalgia and Morton’s neuroma — which each have numerous causes of their own.
The long bones in your feet that attach to your toes are called metatarsals, and when the ends of these bones become aggravated and inflamed, ball of foot pain ensues! What’s behind this irritation?
This occurs when a nerve that runs between the metatarsal bones becomes thickened due to irritation. The result is numbness, tingling, burning, and pain in the ball of your foot, most often (but not always) affecting the area between the third and fourth toes.
Metatarsalgia and Morton’s neuroma are often found together, but can luckily be treated conservatively, with rest, a switch to roomier, lower-heeled shoes, orthotics, and breaking up activities with low-impact options like swimming and yoga. If these methods fail to provide relief, nerve decompression surgery may need to be considered. If you are struggling with ball of foot pain, call our Bloomington, IN office for an appointment today by dialing (812) 333-4422. We can get you the help you need!
 Are you participating in the Walk to End Alzheimer’s on Sept 24 here in Bloomington? What a great charitable cause and excuse to get out there and get some exercise! Of course, if it feels like you have a pebble in your shoe every time you go walking, and when you stop to dump it out, nothing’s there, well, that can definitely be annoying and take away from you walking enjoyment! It also just happens to be a signature symptom of Morton’s neuroma and an associated condition called metatarsalgia.
Are you participating in the Walk to End Alzheimer’s on Sept 24 here in Bloomington? What a great charitable cause and excuse to get out there and get some exercise! Of course, if it feels like you have a pebble in your shoe every time you go walking, and when you stop to dump it out, nothing’s there, well, that can definitely be annoying and take away from you walking enjoyment! It also just happens to be a signature symptom of Morton’s neuroma and an associated condition called metatarsalgia.
Morton’s neuroma is the swelling of a nerve in the ball of your foot, most often between your third and fourth toes. It can feel like your sock is wadded up or a pebble is stuck in your shoe. It can also aggravate the long metatarsal bones that connect your foot to your toes, causing additional pain and inflammation in the ball of your foot.
Luckily, there are ways you can prevent that “pebble in your shoe” feeling and do all the walking you please, pain- (and pebble) free!
If these prevention tips don’t seem to provide any more relief than dumping out the contents of your shoe or adjusting your sock, don’t hang up your walking shoes just yet! Nerve decompression surgery could be just what you need to relieve symptoms. Find out more about this by giving us a call. You can reach our Bloomington, IN office by dialing (812) 333-4422 and we’ll be happy to “walk” you through it!
Sometimes it’s worth taking a risk – having a picnic despite the chance for rain, or heading to the theater opening night in hopes that tickets won’t be sold out. However, there are times when you shouldn’t take chances, and knowing risk factors could help you avoid major problems. This is especially true when it comes to your health, including the health of your feet, and conditions like foot drop.
Are you at risk for foot drop? This condition, also called drop foot, is characterized by an inability to pick up your foot when you step, thus forcing you to drag your toes. The source of the problem can be a nerve or muscular disorder like, polio, ALS, or multiple sclerosis (which is why it’s so important to seek treatment), but it does result from other causes as well. Knowing the risk factors of foot drop, can allow you to watch for symptoms, catch the problem early, and get the prompt treatment you need. Reference this list of risk factors to find out if foot drop could happen to you:
If you recognize a risk factor and are concerned about drop foot, come in for an appointment so we can assess your foot and determine if treatment is necessary. You can contact our Bloomington, IN office by dialing (812) 333-442, or you can use our online contact form to reach us. Catch foot drop before it drags you down. If you think you are at risk, call us today!
This is the time of year when the evenings are warm but comfortable – perfect for taking a stroll after dinner and enjoying the last of the summer nights. However, if your foot feels weak, even taking a nice walk likely sounds far from pleasant. When you have weakness in your feet, it can interfere with activities you enjoy, as well as everyday life, but determining what’s behind that weak feeling will allow you to address it and get you back to doing the things you love.

Sometimes, when feet feel weak, and especially if this causes you to drag your toes, it is a sign of foot drop — also called drop foot — which is a symptom in and of itself of a muscle or nerve disorder or injury. This can stem from diabetic neuropathy, tarsal tunnel syndrome, Charcot-Marie-Tooth disease, multiple sclerosis, muscular dystrophy, and other disorders or diseases that affect your muscles and nerves. Because there are so many sources of the problem, it is vital to determine the underlying issue in order for the appropriate treatment plan to be put in place.
In addition to treating the source of your weakness, managing drop foot symptoms (like feet that feel weak) may also include supportive orthotics, splints, or braces, strengthening exercises, and nerve stimulation therapy to encourage nerve cell repair and regrowth. If damaged nerves and muscles are not responding to these methods, surgical procedures may also be considered.
If weakness in your feet is stopping you from enjoying summer strolls and other pleasures in life, it’s important to schedule an appointment as soon as possible. We will diagnose and treat your problem and help you manage foot drop so you can walk with ease. Dial (812) 333-442 to reach our Bloomington, IN office, and we will be happy to help.

It won’t be long for before kids head back to school, dragging their feet every step of the way! Sure, they might be reluctant to say goodbye to their care-free summer days, but when your feet are literally dragging, that’s a sign of an underlying issue that can be much more serious than the back-to-school blues.
Difficulty picking up your foot (or both feet) when attempting to walk – a condition known as foot drop or drop foot — is actually a symptom of an underlying problem or injury that has affected muscles or nerves. The foot becomes weakened or paralyzed, making it difficult to move it forward. Dragging your toes, slapping the front of the foot down, and compensating by swinging your leg or raising your knee higher when you step, are all signs of foot drop. If you notice any of these symptoms, a visit with Dr. Kevin Powers is important to determine the exact underlying cause so proper treatment can begin as soon as possible.
Although treatments for foot drop vary depending on the source of the problem, typically it is treated with braces or splints and orthotic shoe inserts to provide support, as well as physical therapy exercises to strengthen muscles and help with range of motion. Nerve stimulation can sometimes help as well, and in some cases, surgery may be needed to address nerve damage or bones and soft tissues not responding to conservative care. Treatment will also entail addressing the underlying cause, so it’s essential to have your feet assessed at the first onset of symptoms.
In other words, if you think you have drop foot, don’t drag your feet to make an appointment! Call right away to get the help you need so you can back-to-school shop without a problem! Contact our Bloomington, IN office by dialing (812) 333-4422 or by using our online contact form.
During the summertime, your toes are often on display with open-toed sandals and days at the pool. That means it’s more likely you’ll look down and notice changes, like, for example, a bump on your baby toe. Uh-oh! That, friend, could be the beginning of a bunionette, and though smaller in stature than its big brother bunion, it can still be a big pain!
 Bunionettes are basically bunions but instead of forming on the big toe joint, they develop on your little toe joint. The same forces are at work here: an inherited foot structure prone to the problem, and outside pressure (typically from too tight of shoes) encouraging the toe to drift out of alignment, forcing the joint outward and the toe inward. The more pressure placed on the little toe joint, the worse the bunionette gets, and the worse it hurts!
Bunionettes are basically bunions but instead of forming on the big toe joint, they develop on your little toe joint. The same forces are at work here: an inherited foot structure prone to the problem, and outside pressure (typically from too tight of shoes) encouraging the toe to drift out of alignment, forcing the joint outward and the toe inward. The more pressure placed on the little toe joint, the worse the bunionette gets, and the worse it hurts!
Because bunions and bunionettes are similar conditions, they have similar solutions. You can decrease pain by using padding for a layer of protection between your toe and your shoe. Speaking of shoes – make a switch! Replace narrow, tight footwear with shoes that offer wide, deep toe boxes so toes aren’t squished. Slipping some orthotics inside can help redirect pressure away from your little toe joint, too. There are also stretches you can do and splints you can wear at night to help keep your toe in proper position. Again, like bunions, if these tactics fail to relieve your pain and slow progression, surgical procedures may be considered.
If you notice a bump on your baby toe, don’t let it go – if you do, it will only get worse! Call us so we can assess your condition and determine a treatment plan that works for you.
You can reach our Bloomington, IN office at (812) 333-4422. In the meantime, better sweat the small stuff! Make sure those sandals of yours aren’t adding to the problem and making your little bunionette a big pain.